How periodontal recession develops
Periodontal recession refers to receding of the gums accompanied by exposure of the root surface, and can in principle occur on all dental surfaces. Usually, recessions are the result of toothbrush trauma in the case of patients with "thin gums". In other words, there is often a predisposition for this particular biotype, in which not only are the guns relatively thin, but also the bony support structure underneath is often not intact or is missing to a great extent. If a patient of this type applies the wrong, i.e. highly abrasive toothbrush technique, this mechanical trauma provokes recession of the thin gums and exposes the root surface. But crooked teeth can also cause periodontal recession. For example, if a tooth comes through outside the row of teeth, it is often insufficiently surrounded by firm gum from the very start.
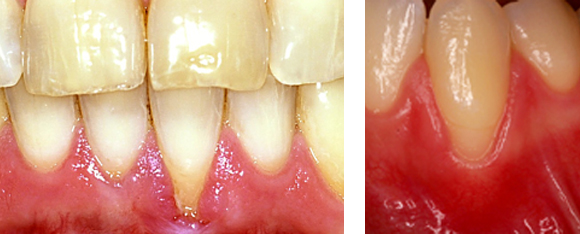
Examples of periodontal recessions:
However, the causes of periodontal recession also include badly fitting dental restorations. Finally, recessions also occur in the context of periodontitis, since the position of the gum margin may adapt to periodontitis-related bone deterioration in the course of the disease. In other words, the gums may recede, causing the depth of the pockets to be slightly reduced (self-limiting effect of periodontitis). Moreover, this effect also occurs during the treatment of periodontitis - as "healthy downsizing" so to speak. The process can also be compared to the subsidence of a swelling. The pocket depth is reduced at the cost of a periodontal recession.
In addition to causing a disharmonious gum line, recessions are also often associated with oversensitivity of the root surfaces, and also sometimes with an increased risk of root caries. In extreme cases, the whole section of firm gum can be lost, leaving only the flexible oral mucous membrane to contain the highly exposed neck of the tooth. In such cases, even barely adequate oral hygiene is virtually impossible.
Necessity of treatment and available treatment options
The necessity of treatment and the prognosis for root surface coverage must be discussed individually in each specific case. Whether treatment is deemed necessary depends not only on the medical condition but also on the aesthetic needs of the patient.
Smaller recessions in patients with good and atraumatic oral hygiene and without complaints or increased risk of caries do not necessarily have to be treated from a medical standpoint. However, if a progressive recession of the gums threatens to compromise oral hygiene and thus increase the risk of infections, treatment may well be deemed necessary.
Basically, exposed root surfaces can be treated non-surgically and surgically. Non-surgical treatment alone, however, has only a palliative relevance in terms of the goal of complete root coverage. In other words, a coverage of exposed root surfaces cannot be achieved, and if it can, then only incipiently. On the other hand, non-surgical treatment can hinder the advance of a periodontal recession and limit the potential damage. Such approaches include changing toothbrush technique over to an atraumatic, non-abrasive technique using a soft toothbrush, and also treatment of oversensitivity (using desensitising medicaments) or, if required, filling therapy for root caries.
In contrast, surgical treatment aims at coverage of the exposed root surfaces. The prognosis for such coverage depends on various factors. For example, there is so far no predictable technique for coverage of periodontal recession in the contact zone between two teeth (interproximal recessions), while the prognosis for specific treatment of receding gums in the outer, visible zones of a tooth (vestibular recessions) may well be good.
Generally, for the coverage of exposed root surfaces we use transposition surgery, transplantation and combinations of both. For soft tissue transplants, transplants of both mucous membrane and connective tissue from the hard palate are used. Today, mucous membrane transplants have only a secondary significance, although there are individual cases where they may (or must) be used as the only available therapy option.
Transposition surgery puts us in a position the cover exposed root surfaces. We often combine this technique with connective tissue transplants, which serve as a sort of underlay. This has the advantage that not only coverage is achieved, but also a thickening of the tissue, which in turn increases the resilience of the result.
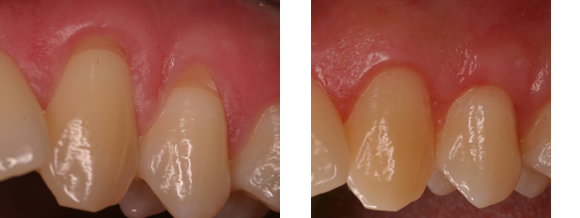
Example of coverage of a recession using transposition flap surgery and connective tissue transplantation:
Nowadays, special innovative techniques allow us the option of inserting connective tissue transplants without opening flaps, in the form of so-called tunnelling techniques. This way, relief incisions are not necessary, so the blood supply is not interrupted in the surgical field and, as a result, the wound heals better and the scar formation that often occurs with flaps can be avoided.
Finally - as in the case of regenerative periodontitis therapy - biological agents can also be used for the coverage of exposed root surfaces. Although it is still too early to have sufficient long-term results, transposition flap surgery in combination with enamel matrix proteins or growth agents would seem to improve the results of root surface coverage.
Example of the coverage of a periodontal recession via transposition flap surgery and enamel matrix proteins:
