Full Mouth Disinfection
Constantly growing knowledge about the influence and the organisation of microbial plaque leads to new approaches in the treatment of periodontal diseases. Periodontitis is a so-called opportunistic multi-bacterial infectious disease. This means that in a healthy oral cavity there are a multitude of bacteria which do not under normal circumstances have a pathogenic effect. But under suitable local and systemic conditions, these germs can become pathogenic. However, there are also a few types of bacteria in the oral cavity with characteristics typical of permanently pathogenic bacteria.
In a case of periodontitis, what we are dealing with is a multiple spectrum of bacteria (biofilms), of which some are strongly pathogenic (i.e. particularly aggressive) and may actually in some cases actively penetrate the soft tissue. Most of these germs have a thoroughly infectious, i.e. contagious character. The resettlement of periodontal bacteria on previously treated root surfaces has been more closely investigated in the last 10-15 years. We now know that, just a few weeks after a conventional treatment of the root surfaces, the number of bacteria in the periodontal pocket has usually climbed almost back to its original level, but that the germs are not as pathogenic as they were before. However. if strongly pathogenic germs re-establish themselves, the pathogenic effect may sometimes start again after a certain period of time and cause new inflammatory changes.
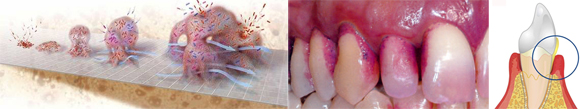
It is important to remember that, in certain cases, in spite of root surface treatment, inflammatory activities may reoccur due to new infections by pathogenic bacteria. Such mechanisms are, of course, dependent on the general immune system of the patient and on external factors.
In recent years, the search has been on for effective strategies to prevent such re-infection and thus to stabilise the effects of the treatment. These include not only intensive follow-up treatment ("supportive periodontal therapy "), but also newly established concepts like so-called "Full Mouth Disinfection".
What is "Full Mouth Disinfection"?
Full Mouth Disinfection" (FMD) is a combination of non-surgical periodontal treatment with accompanying pharmaceutical therapy according to a special concept designed to prevent re-infection of the treated pockets.
This concept is based on four approaches:
1. After periodontal pre-treatment - in contrast to conventional therapy - the root surface treatment of all pockets is carried out within 24 hours to prevent cross contamination by bacteria from not yet treated regions into periodontal pockets that have already been treated.
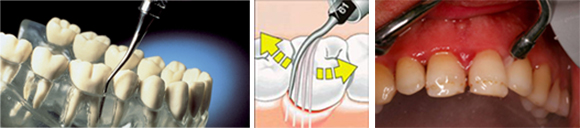
2. Furthermore, the concept includes a comprehensive disinfection of all treated periodontal pockets as well as the whole oral cavity. i.e. the surface of the tongue, the mucous membrane inside the cheeks (buccal mucosa), all of the recesses and niches in the vicinity of the teeth, the soft palate tissues including the palatine tonsils, and other areas. As it is a proven fact that the germs responsible for periodontitis also "hide" in these regions and may from there re-infect previously treated periodontal pockets, the idea is to eliminate all these potential sources of infection.
3. The subsequent "home care" stage requires the patient to actively support prevention of re-infection by means of antimicrobial agents in the form of rinsing solutions, sprays and/or gels. The exact selection of the appropriate agents as well as the manner and duration of their application is individually prescribed according each particular case.

4. Finally, this concept also calls for treatment of the patient's partner, should the partner have periodontitis that needs treatment. Since periodontitis is, as has been emphasised above, an infectious disease, a non-treated partner also represents a potential source of re-infection.
What are the advantages of "Full Mouth Disinfection"?
Merely the root surface treatment of all pockets within 24 hours ("Full Mouth Rootplaning") has in some publications been falsely equated with the original method of "Full Mouth Disinfection". However, on its own, this single therapy seems to have little or no real advantage. In contrast, the overall concept of FMD with all four therapeutic approaches (see above) has several advantages:
In cases of advanced periodontitis, more effective reduction of pocket depth and a greater reduction of pathogenic bacteria can be expected after an FMD than after conventional treatment. This has been verified in a range of studies into the effectiveness of FMD. The FMD procedures enable the results achieved through therapy to be sustained in the long term. In many cases, this also reduces the necessity of later surgical interventions.
Furthermore, we now know that there is also a positive effect on the general state of health. In the meantime, periodontitis has been recognised as a potential risk factor for cardio-vascular diseases, since the bacteria and the inflammation products of periodontitis may have a serious impact on the blood vessels via the bloodstream. The risk of suffering a heart attack or a stroke as a result of periodontitis can be reduced through systematic and lasting treatment of the periodontitis. Another known advantage of intensive periodontal treatment in the form of FMD is that, after FMD, the elasticity of the blood vessels improves significantly, so this concept achieves a much greater reduction of the risk of atherosclerosis than conventional therapy.
To sum up, FMD is a modern concept for non-surgical periodontal therapy which - if all its components are consistently applied - can be expected to yield more favourable therapy results than conventional periodontitis therapy. The FMD concept is, therefore, an integral part of the systematic periodontal therapy that we conduct in our Dental Clinic.