Regenerative periodontal therapy
Periodontitis is associated with a loss through inflammation of the periodontal structure that supports the teeth (the periodontium). This process also involves deterioration of the bone surrounding the teeth. The highest priority in periodontology is to eliminate the inflammation and to restore the original, intact state of the periodontium.
Conventional, "open" approaches to periodontitis therapy involve cleaning the root surfaces under visual control by means of a so-called flap operation followed by stitching the gum again tightly over the cleansed defect. Even if the originally increased pocket depth may be reduced, in comparison to regenerative procedures these approaches are moderate and are primarily aimed at a reparative rather than regenerative form of healing.
In contrast, the aim of regenerative approaches goes beyond merely reducing pocket depth and also includes the restoration of all lost periodontal tissue. However, so far a complete, genuine regeneration is something that has rarely been described in the literature. Nevertheless, periodontology today has a range of established methods at its disposal with which the lost support tissue and thus the bone itself can be regenerated.
Apart from transplantation of the patient's own bone volume (autologous bone transplants), there is also the possibility of using bone replacement materials for the restoration of periodontal bone defects. These are either produced synthetically or derived from animal bones, sometimes also from coral. As a rule, the material introduced into the bone defect serves as an absorbable matrix into which the patient's own bone can grow. Some materials are also reported to have bone growth stimulating properties. Depending on the material introduced, its absorption may be more or less swift and effective.
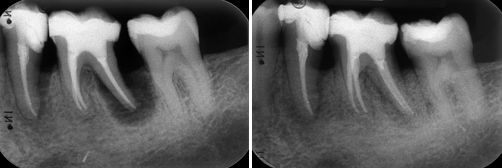
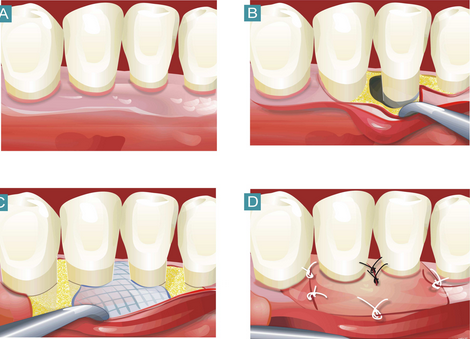
Example of the application of bone replacement materials:
Another technique is Guided Tissue Regeneration (GTR). Here, a mechanical barrier membrane is used to separate the soft tissue from the pocket of the cleaned bone defect in order to keep the space open for a regenerative healing of the bone defect. In the meantime, a whole range of absorbable and non-absorbable membranes have become available. Because, in comparison to non-absorbable membranes, the absorbable varieties do not need to be removed and tend to be less susceptible to complications, they are the membranes more often used nowadays. A basic distinction is drawn between synthetic and collagen membranes. Depending on the extent of the defect, bone replacement materials are quite often used in combination with membranes.